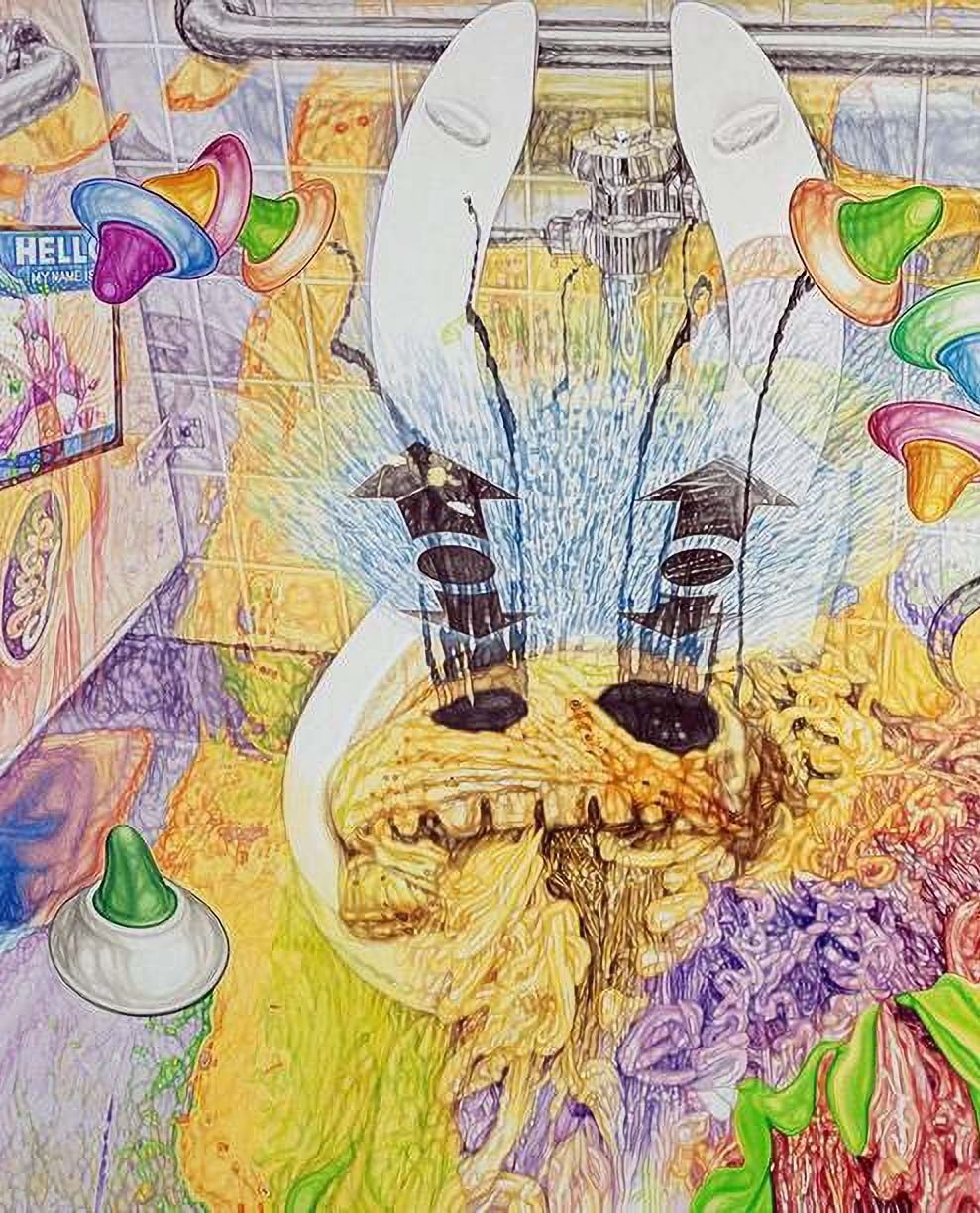
My unofficial Vital Study Zine #14 with observations from Vital Psychedelic Training and recent happenings in the space
Dr Ben Sessa’s book The Psychedelic Renaissance acted as exactly that.
The agenda for a new Albion is effectively a ‘hypersigil’ – the gnostic term for a creative work that somehow manifests its content. These effects even included the buzz phrase the proceeding new era of research was awarded.
Debuting a decade ago, The Psychedelic Renaissance contained ideas Sessa first officially voiced in a presentation to the Royal College of Psychiatrists in 2006. LSD hadn’t been mentioned in its halls for over 30 years.
Since The Psychedelic Renaissance took psychiatry by storm Dr Sessa has hardly been flouncing around in a kaftan. He’s living the experience, conducting frontline child trauma and addiction treatment… including acting as lead psychiatrist on the Bristol Imperial MDMA for Alcoholism (BIMA) project, where patients relapsing into heavy drinking were cut to a rate of 21% from the 73% who do so despite trying medications, 12-step and conventional therapy.
BIMA research took place at leading clinic Awakn, co-founded by Sessa in Bristol, UK. It’s now listed on the NEO Toronto stock exchange and has hooked up with David Nutt’s Drug Science. The Mithoefers are on Awakn’s advisory board. Celia Morgan is head of ketamine assisted therapy, an area where Awakn just received 66% of new funding from the UK government and licensed its staggeringly successful ‘Project Kestrel’ design to US chain Revitalist.
“I resent the assumption this is all about money. My job is getting the maximum amount of psychedelics to as many people as possible”
Sessa is an avid member of the psychedelic ‘subculture’ too. In 2015 he co-founded and ran the Breaking Convention conference that showcases the space’s sharpest upcoming minds. His children are named Huxley, Jimi and Kitty.
I’ve noticed during academic presentations that after their personal intro is over it’s de rigueur for presenters to, if they’d like, admit to any horrendous biases.
Prostrate before you, I make clear: Dr Sessa is my age, lives and cheerleads for my home town, and confesses to an achingly middle class upbringing that includes winter sports and bedroom DJing… so there’s ‘similarity bias’ there. Moreover: only in the past few weeks I discovered he wrote a column for a hipster magazine I was founding editor of that’s having a bit of a moment now, and made a cameo in a Channel Four sketch show I wrote on.

So don’t ask me to justify statements like ‘Sessa is our generation’s admittedly unlikely Leary or McKenna’, and yes, I am calling that with this blog post. Instead ask Vital students, whose reactions to Dr Sessa ranged from “That was my favourite presentation so far” to “You’re the most interesting person to hear from in psychedelics right now” and “This has me so excited and hopeful for the future of this space!”
Whilst actually being the closest thing we do have to Timothy Leary or Terrence McKenna – closest rival Robin Carhart-Harris has recently zhuzh’d up his look just to keep up – Sessa has succeeded in ushering in a revolution where the two counterculture icons failed.
“This is the psychedelic era. Here. Now. We’re living in it,” he decrees to Vital’s class of ‘22.
“Following medicalisation the psychedelic underground is richer and freer than ever”
How has Sessa made this happen? By following his own advice in the closing pages of The Psychedelic Renaissance.
‘An unfortunate but necessary truth is that professionals working in this field must remain as boring and staid as possible,’ he solemnly advised in those very pages, ‘as well as inspirational and enthusiastic – to get the message across. I do not say all of these dull and conservative things because I lack imagination or fail to appreciate the fun, wonder and spirituality of the psychedelic experience. On the contrary, I welcome and embrace it.’
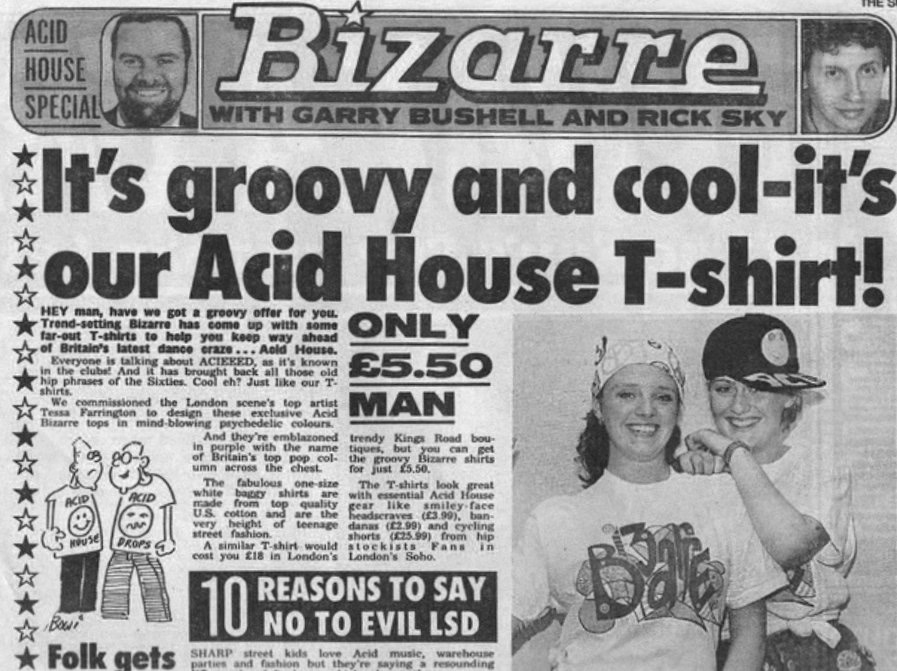
This trademark approach of blowing minds by stealth doesn’t stop him racking up a ton of newspaper credits, where he lays down psychedelic law (and lore) in a fashion also quite dissimilar to his predecessors.
In fact, only this year at 2022’s Breaking Convention he decimated criticisms of corporadelia at his £6K per programme Awakn clinics with: “I resent the assumption this is all about money. My job is getting the maximum amount of psychedelics to as many people as possible, and researching that is very costly. There will still be raves, festivals, ceremonies. The psychedelic underground is richer and freer than ever post-medicalisation.”
Dr Sessa is a boon to journalists. Here’s a few choice quotes from his week fourteen Vital lecture:
“There’s nothing more dangerous than drinking a bottle of vodka a day”
“Then they go back on heroin, or other far, far more dangerous substances like alcohol”
“Three quarters of a million people in the UK take ecstasy every weekend and our hospital wards are not full of casualties”
“I’m not that spiritual a guy, but I’ll talk to patients about kundalini and chakras till the cows come home. They do also want to talk about things like how to get their children out of social services care”
Here he is on NBC with MAPS’ The Mithoefers talking about their slot on Netflix’s How to change Your Mind, showing ITV viewers around Awakn, plus watch his TEDX Talk on psychedelics as antibiotics, explain childhood trauma and MDMA therapy and more on the New Psychonaut YouTube lecture archive.
Here’s this issue’s contents arranged along Vital Psychedelic Training’s five learning themes:
















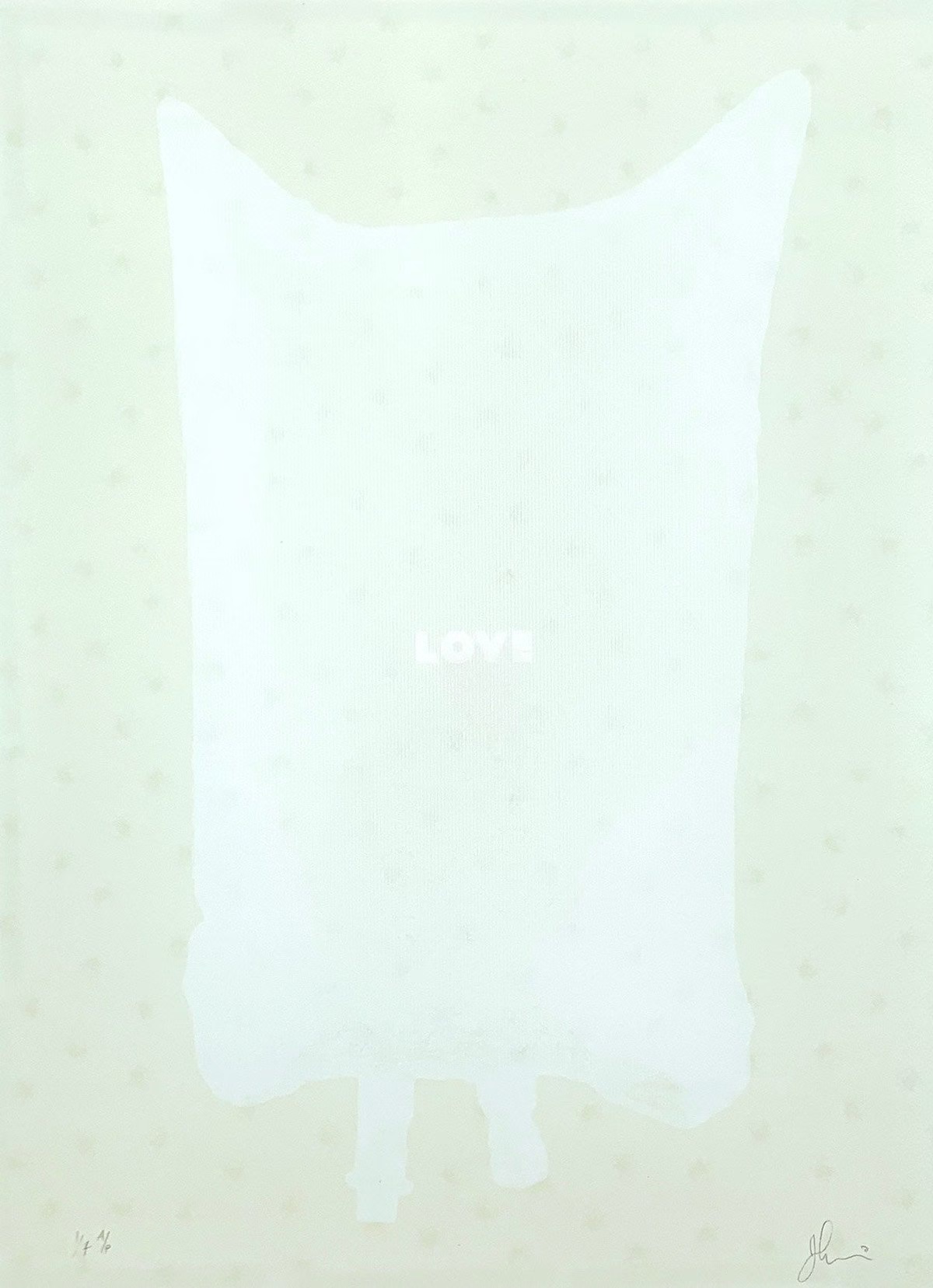










Psychedelics are the psychic antibiotic.